TL;DR–Healthcare burnout, characterized by emotional exhaustion, depersonalization, and diminished professional fulfillment, originates from medical education's shift towards scientific rigor. Balancing Abraham Flexner’s efficiency-driven reforms with William Osler’s emphasis on patient-centered compassion can effectively address today's growing burnout crisis.
Key Takeaways:
- Healthcare burnout has surged among medical professionals.
- Flexner’s scientific rigor has inadvertently fostered environments prone to burnout.
- Osler’s compassion-driven approach provides viable solutions to this crisis.
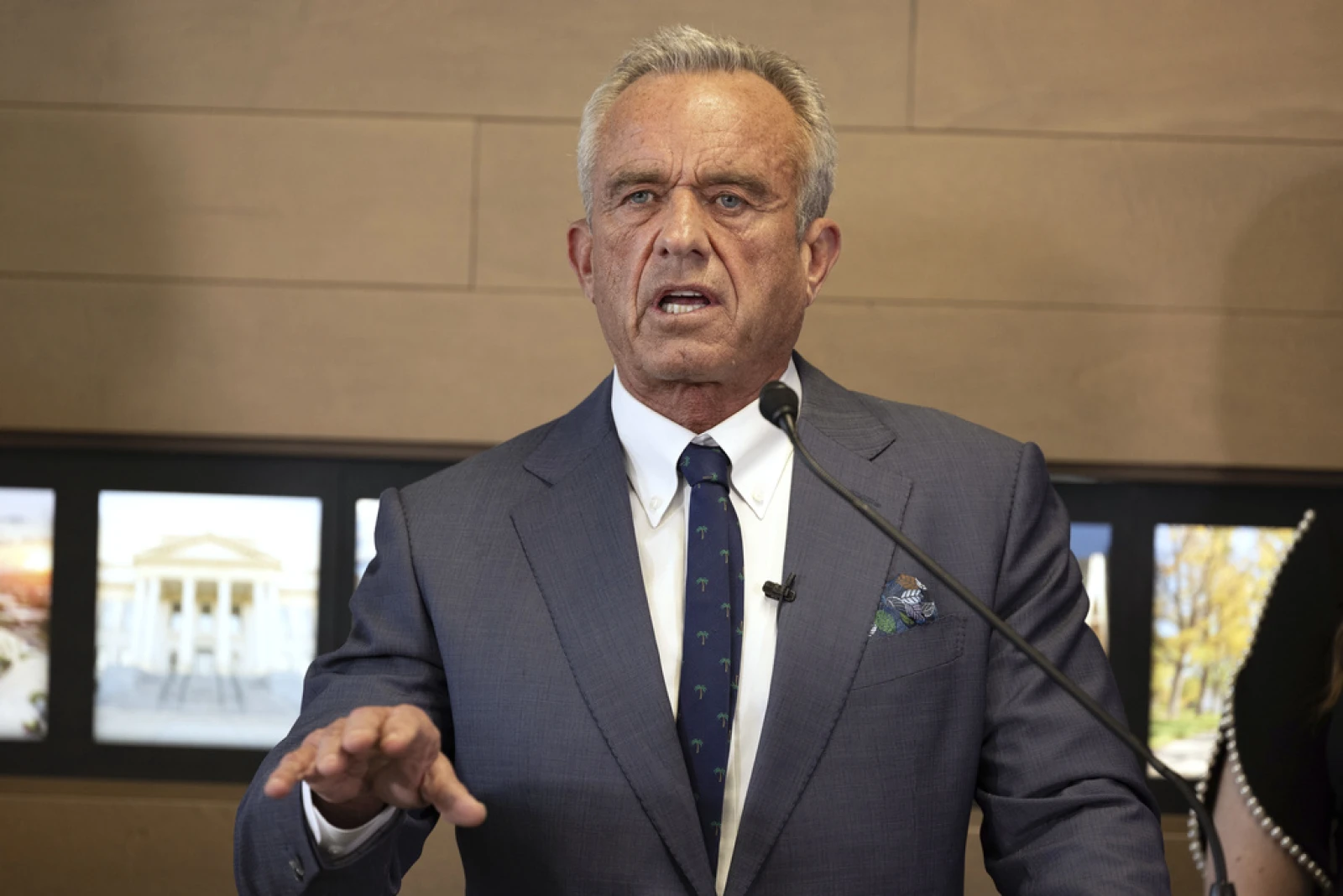
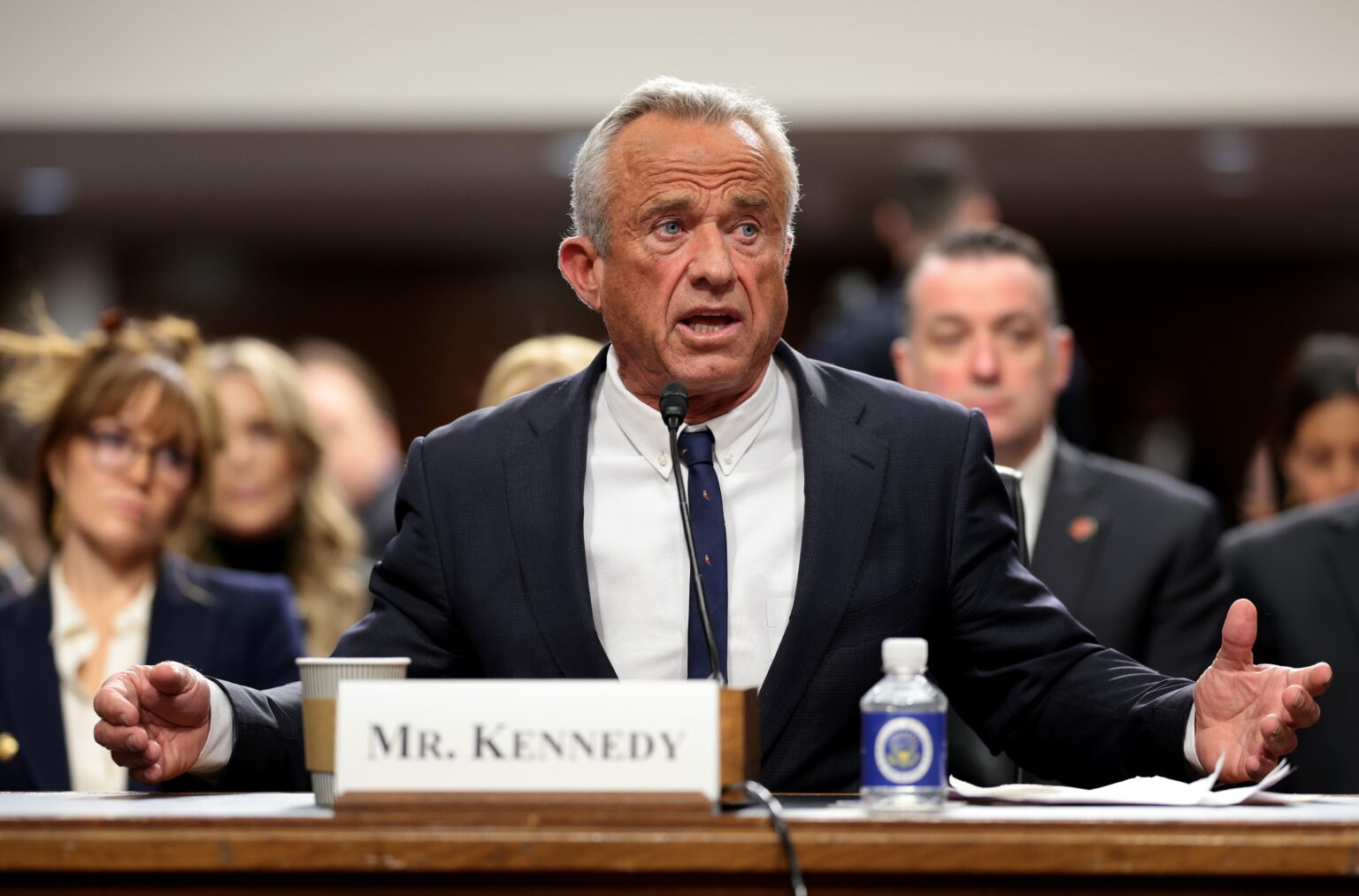
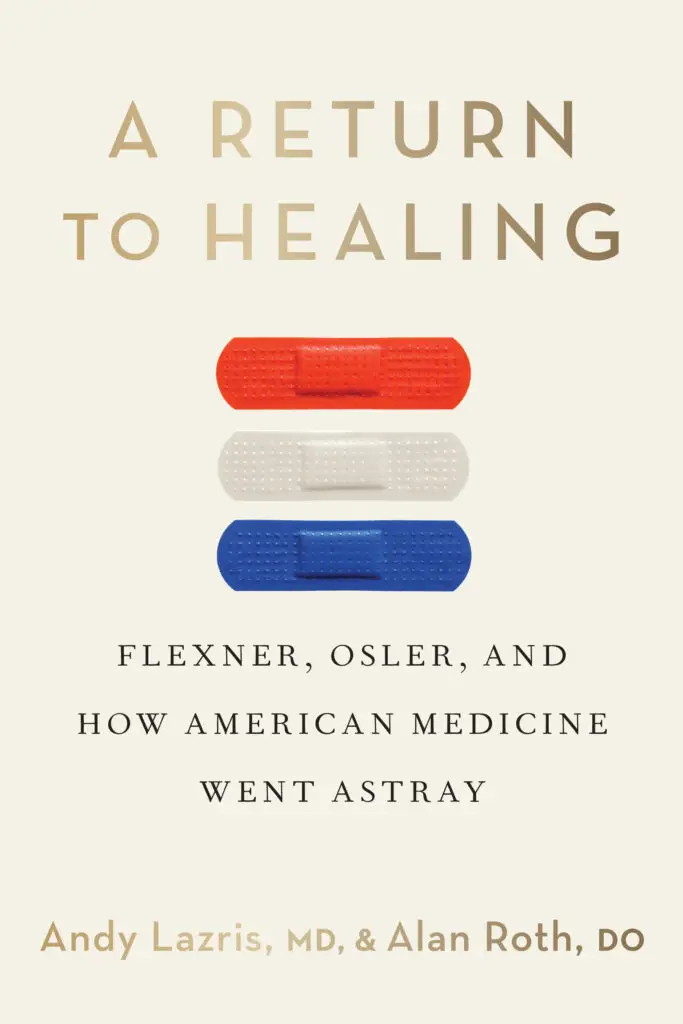
Healthcare burnout has reached critical levels, profoundly impacting medical professionals and care delivery across the globe. A deeper historical understanding, specifically examining the influences of Abraham Flexner and William Osler, sheds important light on how we arrived at today’s crisis. Guided by insights from A Return to Healing, we uncover why the balance between scientific efficiency and compassionate patient care is essential.
Defining the Crisis: Healthcare Burnout
Burnout in healthcare is increasingly common and characterized by symptoms including emotional exhaustion, depersonalization, reduced professional satisfaction, and decreased quality of patient care. Recent data reveals dramatic rises in searches for terms like “healthcare burnout symptoms” and “causes of healthcare burnout,” highlighting widespread concern within medical communities and validating the experiences of healthcare workers.
The Flexner Factor: Efficiency, Rigor, and Burnout
Abraham Flexner’s transformative 1910 report fundamentally altered medical education by enforcing strict scientific and academic standards. While Flexner’s reforms significantly improved medical competence and education quality, these benefits came with a cost. The intensive focus on scientific rigor led to demanding workloads, depersonalized clinical environments, and diminished opportunities for meaningful patient interactions.
Today, healthcare professionals often face environments that prioritize productivity and efficiency over meaningful patient engagement. This shift has intensified workloads, increased administrative burdens, and diminished job satisfaction—all contributing significantly to burnout.
Osler’s Alternative: Compassion as Prevention
In sharp contrast, William Osler advocated for medicine as an inherently compassionate and humanistic practice. Osler emphasized bedside teaching, direct patient engagement, empathy, humility, and prioritizing patients’ emotional well-being alongside clinical outcomes.
Osler’s methods have clear advantages in addressing burnout. Physicians who maintain empathetic, humanistic interactions with patients report greater job satisfaction, increased emotional resilience, and reduced burnout symptoms. Modern research consistently supports Osler’s ideas, revealing that compassionate care not only benefits patients but significantly enhances professional fulfillment and reduces burnout risk for caregivers.
Connecting the Past to Present Realities
Today’s healthcare burnout crisis is directly linked to historical shifts set in motion by Flexner and counterbalanced by Osler. Common search queries like “Why is healthcare burnout increasing?” reflect ongoing concerns about how modern healthcare structures exacerbate this issue. The drive toward intense specialization, administrative overload, electronic health record burdens, and reduced patient interaction are modern manifestations of Flexner’s original vision.
Healthcare workers today increasingly voice concerns about losing personal connections with patients, which they view as essential to professional satisfaction and quality care. This loss contributes heavily to burnout, reinforcing the need to revisit the compassionate aspects Osler championed.
What Can Be Done? A Return to Balance
To effectively address burnout, healthcare systems must seek a renewed balance between scientific rigor and compassionate patient care, drawing inspiration from Osler’s principles. Practical solutions include promoting manageable workloads, streamlining administrative tasks, enhancing patient-provider interaction, and incorporating mindfulness and empathy training into medical education.
Additionally, institutions that actively encourage a culture of empathy and support have demonstrably lower burnout rates. Policies that facilitate meaningful interactions, such as more patient-centered scheduling and protected clinical time, directly address the roots of burnout, creating healthier, more satisfying work environments.
To further explore the historical roots and modern solutions for healthcare burnout, subscribe to our YouTube channel and watch our in-depth companion video below. For a more comprehensive understanding, order A Return To Healing. Join our mailing list to participate in ongoing discussions, exchange ideas, and receive additional resources on effectively addressing burnout in healthcare.
Healthcare Burnout Explained—The Flexner and Osler Legacy
Curious to see how history shapes today’s burnout crisis? Our companion video unpacks the legacies of Abraham Flexner and William Osler—two medical giants whose opposing philosophies still impact doctors and patients alike. In just a couple minutes, discover how the roots of healthcare burnout go deeper than long shifts and paperwork, and why finding the right balance between science and compassion remains urgent for the future of medicine. Watch below to learn more, and join the ongoing conversation about what real healing should look like.