A borderline blood sugar reading shouldn’t lead to anxiety, overmedication, or unnecessary doctor visits—especially in older adults. Yet for millions of people, that’s exactly what the diagnosis of prediabetes has triggered.
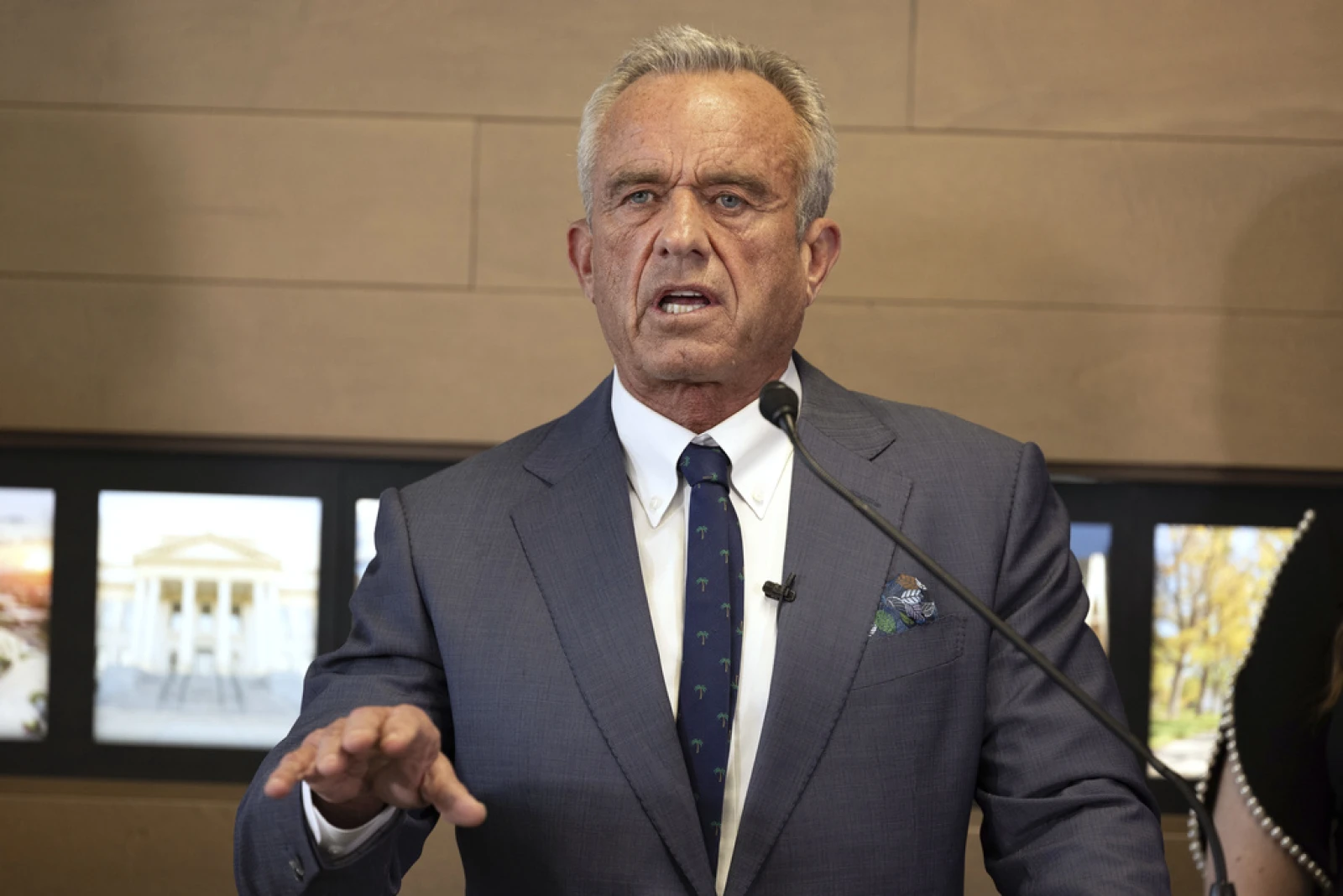
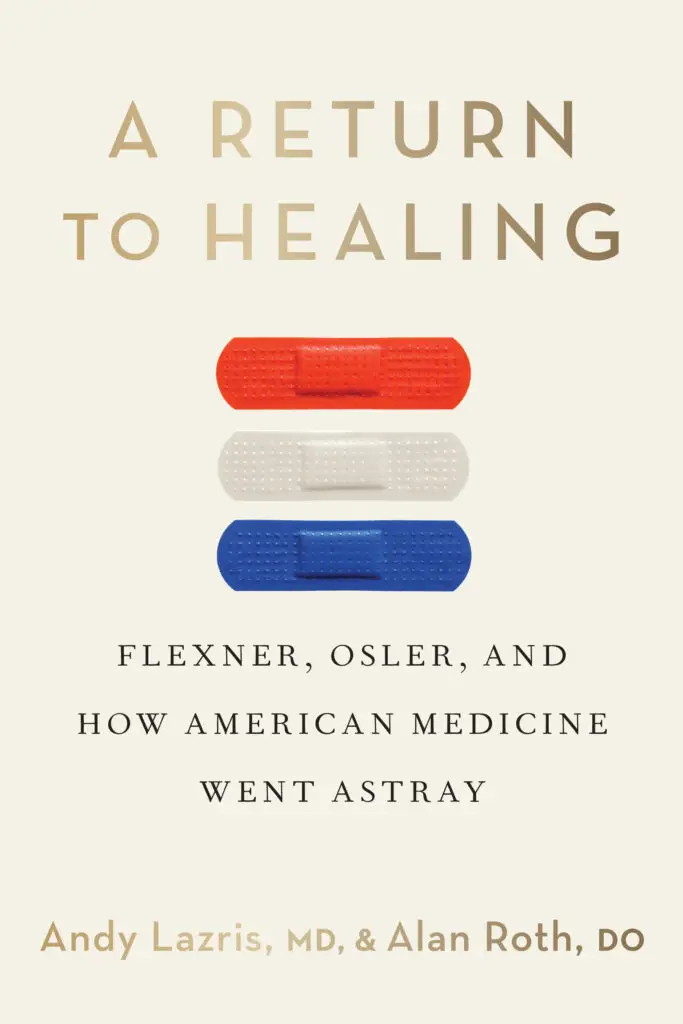
In this insightful article from American Family Physician, Drs. Andy Lazris and Alan Roth examine the real-world implications of prediabetes in older adults, where the risks of labeling and overtreatment may outweigh the benefits. Drawing from data, patient experience, and current guidelines, they challenge the notion that prediabetes is a meaningful or actionable diagnosis for most seniors.
Prediabetes in Older Adults: What the Data Really Says
Prediabetes has become one of the most common diagnoses in America—especially among older adults. But what most patients don’t know is that the condition itself is poorly defined, and the majority of those diagnosed will never develop diabetes.
The article outlines how in the early 2000s, the American Diabetes Association lowered the threshold for diagnosis, instantly labeling millions of people with a “condition” that may not be clinically meaningful—particularly in patients over 65. As a result, patients are often pushed into repeated lab testing, lifestyle counseling programs, and even medication without a clear benefit.
For example:
Studies show that older adults with prediabetes often remain stable or revert to normal without intervention.
Only a small percentage progress to type 2 diabetes, and even fewer experience long-term harm.
The diagnosis can trigger fear, stigma, and overtreatment—distracting from more meaningful health goals like mobility, heart health, or fall prevention.
The article stresses that prediabetes in seniors is rarely a call to action. Instead, it’s often a byproduct of disease expansion in medicine—where thresholds are lowered to encourage early detection, even when the evidence for benefit is weak or nonexistent.
A Smarter, More Human Approach to Blood Sugar
This article reinforces one of the key principles from A Return to Healing: health care should focus on what actually improves a patient’s quality of life. For older adults with mild hyperglycemia, the most effective path forward may be simple lifestyle improvements, reassurance, and shared decision-making—not prescriptions or fear.
If you or your patients are navigating a recent prediabetes diagnosis, this resource will help you see the bigger picture and avoid unnecessary harm.