Syncope—brief loss of consciousness—often leads to emergency visits, excessive testing, and hospital admissions. But is that always necessary?
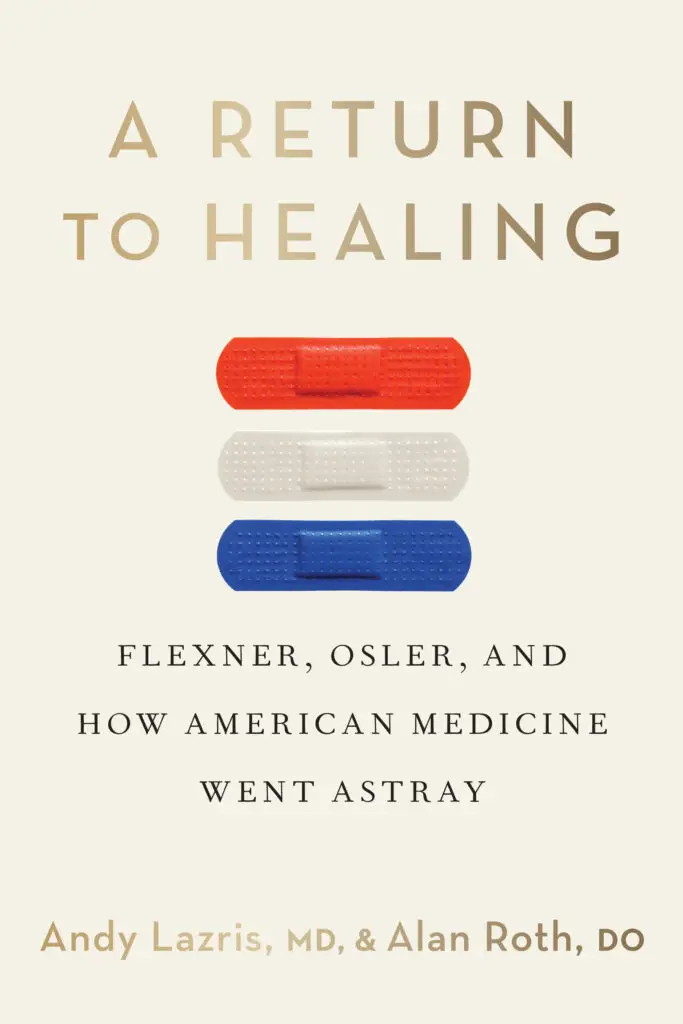
In this article from American Family Physician, Drs. Andy Lazris and Alan Roth offer a smarter, more efficient approach to evaluating syncope in older adults. Drawing from real case studies and current clinical guidelines, they reveal how hospitalizing low-risk patients often leads to costly overuse, diagnostic noise, and preventable harm—without improving outcomes.
Syncope and the High Cost of Overreaction
The case of a healthy 78-year-old who fainted while raking leaves illustrates a common pattern: unnecessary CT scans, hospital telemetry, echocardiograms, and referrals—all adding cost and confusion without clarity. Despite a thorough workup, no cause of syncope was found. After discharge, the patient fainted again—this time with dangerously low blood pressure.
The article shows that:
40% of adults experience syncope in their lifetime
27–35% of emergency department patients with syncope are hospitalized
Most in-hospital tests (CTs, Dopplers, echocardiograms) have low diagnostic yield
Hospitalization increases risk of adverse events—including medication errors, falls, and unnecessary treatments
Annual Medicare spending on syncope admissions exceeds $2.4 billion
Evidence-Based Tools, Not Protocol Overload
The authors recommend using clinical risk stratification tools—like ECGs, targeted history-taking, and physical exams—to determine who actually needs further evaluation. They cite data showing that inpatient testing rarely changes outcomes and often leads to incidental findings that create new (and unnecessary) clinical problems.
A Patient-Centered Approach to Syncope
This article echoes the central message of A Return to Healing: that less medicine, done more thoughtfully, often leads to better outcomes. It encourages clinicians to replace automatic hospital admissions with clear communication, shared decision-making, and careful outpatient follow-up.
Whether you’re a provider, caregiver, or patient, this article offers a practical framework for delivering right-sized care when it matters most.