What the pandemic taught us about medical overuse—and how less care can sometimes lead to better outcomes.
The pandemic disrupted nearly every part of our healthcare system—but one unexpected outcome was the steep decline in unnecessary medical care during COVID-19. With routine checkups, screenings, and elective procedures paused, many patients received far less care than usual. Surprisingly, outcomes didn’t worsen—and in some cases, they improved.
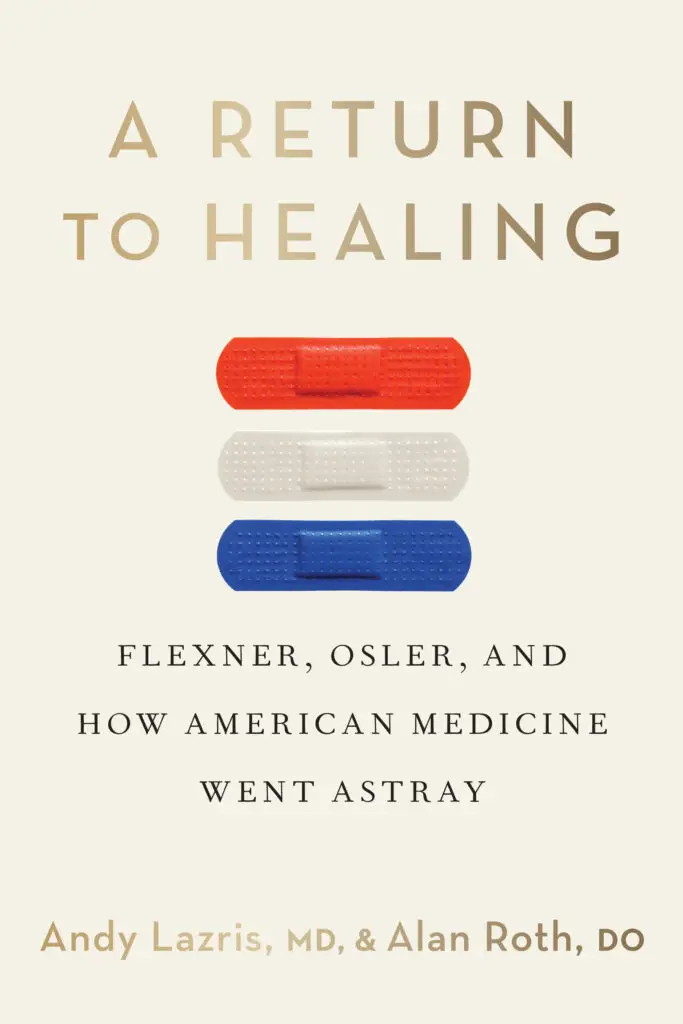
In this compelling article from American Family Physician, Drs. Andy Lazris and Alan Roth reflect on what the pandemic taught us about overuse in medicine—and what we must do moving forward. The reduction in routine visits and procedures gave researchers a chance to assess outcomes when many common (but often unnecessary) tests and interventions were skipped. The findings were striking.
Avoiding Unnecessary Care: A Hidden Benefit of Crisis
The article outlines how up to 20% of U.S. medical care is considered low value, with an annual cost exceeding $300 billion. These include:
ECGs and lab panels during routine checkups
Unnecessary imaging for back pain
Cancer screenings in older adults
Elective procedures with limited benefit
When COVID halted routine care, there was a 46% drop in elective cardiac catheterizations—with no measurable rise in adverse outcomes. This “natural experiment” showed that less medical care can sometimes lead to better outcomes and fewer complications from overdiagnosis and overtreatment.
A Return to Healing: Learning From Crisis
This article connects directly to the message of A Return to Healing: that more medicine is not always better. The pandemic forced clinicians to focus on what really mattered—critical care and urgent needs—and exposed just how much of our day-to-day healthcare might be unnecessary, costly, or even harmful.
If we want to build a smarter, more compassionate system post-COVID, we must resist the urge to return to “business as usual” and instead lean into evidence-based, patient-centered care.